
The power of networks - the story of four hospitals
FEATURE – This article shares the lean journeys of four North American hospitals, and their learning's, reminding us that being part of a network of likeminded practitioners is critical to our success.
Words: Paul Pejsa, Director, Catalysis Healthcare Value Network
When healthcare organizations take the bold step to embark on a lean transformation, the results they anticipate are based on one thing: improving patient outcomes.
At Catalysis we first began helping hospital administrators understand and implement lean principles in 2008, before lean was truly proven in the industry. Dr. John Toussaint, founder and CEO of Catalysis (and a former hospital administrator), used his career experience to bring other hospital leaders along on their own lean transformation journeys.
The Catalysis Healthcare Value Network (CHVN) exists to give healthcare leaders who are interested in lean management systems a place to engage and learn from one another and discuss best lean healthcare practices. More than 70 leaders belong to CHVN, and they eagerly discuss their lean health experiments and successes with each other.
We have been very fortunate to work with so many healthcare organizations, and have learned so much from their work with lean thinking. So we thought it would be interesting for Planet Lean readers to share the work of some of the successful lean healthcare organizations we have worked with, hoping these will help others in the sector to understand how lean could work for them, too.

In 2013, Roger Chen, vice president of Organization Transformation, re-launched lean across Lee Health to identify and reduce waste across the system without cutting jobs or pursuing top-down budget reductions.
Chen drew on his General Electric and Toyota experience to establish a framework using lean tools for process improvement as well as strategy deployment.
The first step was to invite everyone on the management team to read John Toussaint's Management on the Mend, which explains the process and helped create a common understanding of lean principles across the top of the organization. With the support of cross-functional leaders (from Finance, HR, and IT – as well as physicians), Lee Health began getting results that benefited patient outcomes in a very visible way.
For instance, the team created a "Door-to-Needle" lean initiative to ensure ischemic stroke patients who arrive at the hospital are treated with tPA (Tissue Plasminogen Activator) medication as quickly as possible. The positive effects of tPA on patients with acute ischemic stroke are very much dependent on time, with guidelines recommending a door-to-needle time of 60 minutes or less: Lee Health set a goal of treating these patients within 20 minutes (an improvement of more than 50%) from the time of diagnosis. Decreasing the door-to-needle time allowed the organization to improve a patient safety measure and enhance the patient's quality of life.
The organization has benefited in many other ways from its implementation of lean. For example, the system for managing the use of Large Volume Infusion Pumps (LVIP) was improved, introducing a way to monitor where the pumps are at all times. The new system allows the hospital to avoid having to purchase new equipment, while providing safe, reliable LVIP care at all Lee Health locations. In almost two years, Lee Health has not had a single instance of a pump not being available for a patient, which happened regularly before the new process was implemented.
Another result of lean was reflected in Lee Health's work in the Golisano Children's Hospital pediatric intensive care unit (PICU). Lean leaders instituted a kanban system in the supply area that not only reduced the supply cost per patient day by 12%, but also increased the employee engagement scores of the PICU team from 73.9 to 77. The system is now being brought to other departments across Lee Health.
"Lean thinking and principles helped us to simplify the process and problem solve," said Evan Lewis, senior lean specialist at Lee Health. "A wide array of staff was involved in the decision making – from system level executives to nurses and lab technicians to front-line staff. It was a top-to-bottom process." You can view more improvements implemented by Lee Health in this video.
Today Chen and his team look to the horizon to determine what lean can do for Lee Health in the future. "We started four years ago with a blueprint and helped others implement the plan," Chen said. "It's time to create a new blueprint that shows how lean principles will help us evolve to the next level."

Like many large organizations, the Palo Alto Medical Foundation for Health Care, Research and Education (PAMF) had grown into operating silos that didn't communicate effectively with one another and served each patient independently. As a patient, your experience would vary hugely depending on which part or location of PAMF you'd be visiting.
"Internally, we viewed our locations and specialty offerings independently, but our patients see us as one entity," said Martha J. Lauderdale, interim vice president of ancillary services at PAMF. "They want the same experience no matter what location they go to for care."
Following a few attempts of introducing lean thinking, PAMF's senior leadership team conducted a site visit at ThedaCare, a model lean healthcare organization based in Appleton, Wisconsin. The team met with John Toussaint and observed what a lean system looked like. Upon returning to California, they began to realign the primary care delivery system using lean principles and what they had learned from their gemba walk at ThedaCare.
They started with a model cell, tied to key performance targets. The narrow-and-deep model cell approach allowed PAMF to create a new system with standard work to sustain improvement and align everyone on larger organizational goal to transform the patient experience.
One of the initial results of its lean journey was improving in basket management to enhance patient care. Staff at PAMF felt that with more patient engagement, clinicians could more quickly and accurately meet the patients' needs. Additionally, lean thinking helped eliminate staff burnout and fatigue – which had previously been major issues for the organization.
PAMF medical assistants and nurses increased their level of patient engagement and involvement in direct care. Professionals who represent the first line of contact with patients were now in a position to quickly and efficiently identify their concerns and communicate them to physicians, thus speeding up the process of care.
Lauderdale said: "Our new standard work – consisting of medical assistants and nurses partnering with physicians – greatly improved the flow of patient care. This was a significant change that lean brought us: it allowed us to create a consistent, definable patient experience and to establish flow in primary care across adult medicine and pediatrics."

"Our focus is on quality and quality happens at every level," said Debbie Goodwin, Kaizen Learning and Development Consultant at Salem Health. "To transform our culture and implement lean methods that would lead to better quality, we needed to involve everybody."
Unit leaders at Salem Health were trained so they could deploy and use the fundamentals of lean in their respective departments. Concepts including team huddles, visual management boards, four-step problem solving, and standard work were implemented throughout the organization.
Using lean problem solving methodology, Salem Health was able to improve hand hygiene compliance and decrease healthcare acquired infections (HAIs) at the organizational level. In departments, staff participate in problem solving and have enhanced processes, such as how to manage patient financial requests or schedule patients for procedures. In addition, the team created a metrics tracker, used to convert lean improvements (waste removed from the system, time saved and inventory managed) into dollars. "It's not 'hard' dollars in every instance, but it gives us a great way to look at improvements each month from a financial point of view," said Goodwin.
Using the kaizen process, an intake coordinator at Salem Health's Spine Center realized the Center was tracking patient outcomes for both surgical and non-surgical patients – 320 patient outcomes per month. He learned that as a Center of Excellence (COE) the Spine Center only needed to track 60 surgical and non-surgical patient outcomes for a period of 24 months. By following the new guideline, the Center saved nearly $200,000.
Salem Health staff in the Wound Care department had concerns about patients who did not complete background paperwork before their first scheduled appointment, which meant a nurse spent up to 40 minutes assisting the patient at the time of the appointment just to gather the necessary information. First-time appointments generally lasted two hours. Using the lean four-step problem solving process, the team tried to improve the paperwork collection process by committing to calling all new patients the day prior to their first appointment. This took a nurse 20 minutes and 89% of patients were contacted. With this test complete, staff reduced new appointment times to one hour, decreased no shows and patient complaints about needing to do "extra" paperwork.
Lean allowed the hospital to save $36 million.
"Now, whatever comes our way, including reimbursement declines or other changes to healthcare regulations, we know we can adapt using lean principles to meet each challenge," Goodwin said.

After a site visit to observe lean management principles in action, CEO Don Shilton and his leadership team knew they could create their own high-performing lean organization.
"We first established a performance team, trained key people on the new way of thinking, and worked to understand the tools we could use to make day-to-day improvements," said Lydia Chudleigh, who served as vice president of quality, performance and diagnostics at St. Mary's. They started in just two departments, but within six months nearly every department of St. Mary's was huddling each day, discussing staff suggestions and improvement measures.
According to Shilton, a key learning for the hospital's executives was to focus on just a handful of improvements rather than attempting to solve everything at once. They originally had 13 improvement goals, but soon realized they were too many. They moved to seven, then five, and finally four.
"When we invited leaders from Catalysis to help us, our momentum shifted," said Shilton. "We worked with four or five groups at a time, ultimately training everyone in lean principals and tools. This has made all the difference in the world."
One of St. Mary's first lean achievements was meeting its goal to lower the hospital's standardized mortality ratio (the hospital scored the lowest mortality ratio of any hospital in Canada twice in the past five years). There's more: in 2015 the organization set a goal to implement one improvement per employee per year (1,300 in total) and exceeded it. The number of improvements doubled in 2016.
"Most recently we set a goal to reduce patient falls at our facilities by 25%," said Chudleigh. "Lean enabled us to exceed that goal as well. We reduced patient falls by 32% the first year and another 25% in year two, for a two-year reduction of over 50%. Our focus today is on reducing infection rates by 25% and, so far, we've lowered them by 50%. Because of lean thinking, these improvements can be sustained across organization."
One element that, we found, is common to all these lean transformations – and that has surely contributed to their success – is the active and enthusiastic participation of senior leadership. Indeed, we have learned that lean has a higher chance of sticking when it develops as an organization-wide initiative that everybody contributes to – starting with top management.
But there's another important lesson that we have learned by working with so many organizations in the healthcare industry: lean is difficult to get off the ground, and even more difficult to sustain – in fact, organizations often hit something of a "transformation plateau". That is what makes being part of a network so critical.
Having others on the journey to discuss with and benchmark against is fundamental. At the Catalysis Healthcare Value Network, we strive to facilitate this sort of peer-to-peer networking because we believe that being in a community of likeminded practitioners makes us all stronger. When individuals can share ideas, learn from other people's experiments and see what makes lean work in similar organizations, the "virus" spreads much more quickly.
THE AUTHOR

Read more


INTERVIEW – The Lean Enterprise Academy just launched the Lean Learning Journey, an online platform from which practitioners can pull the practical knowledge they need in their lean transformation.


FEATURE – Our coverage of the Covid-19 emergency continues with an article discussing how lean healthcare principles can support and protect the professionals at the front line of this war.
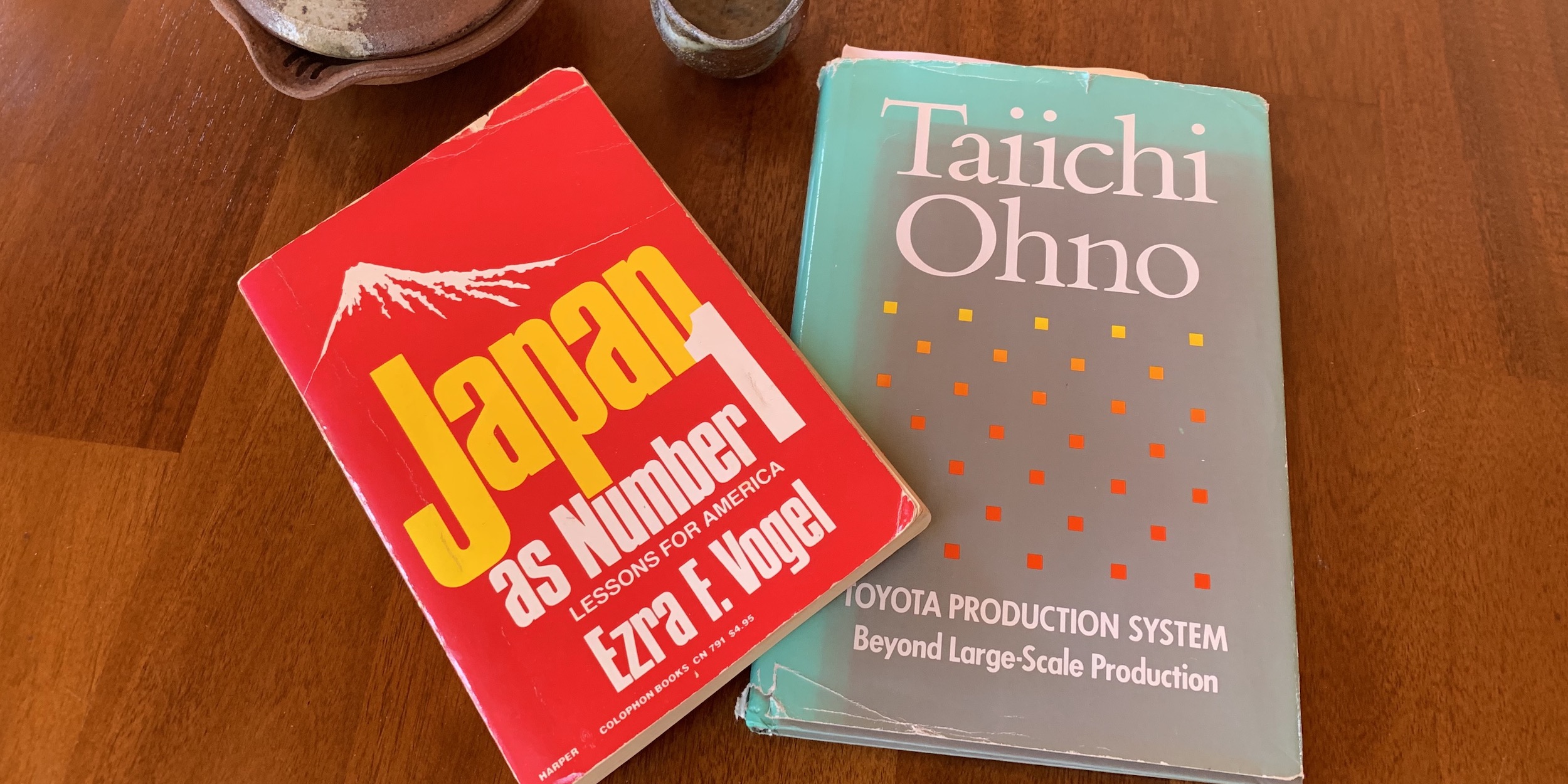

FEATURE – John Shook remembers the work of Ezra Vogel and Norman Bodek and discusses how, in their own way, each of their contributions help us to understand the Toyota Production System.


FEATURE – In the age of complexity and disruption, flowing value to customers as quickly as possible is critical. The new Toyota Flow System strives to address this issue.

