Treating heart attack patients more speedily through lean
FEATURE – Long waiting times are bad for both patients and hospitals, but when we talk about heart attacks reducing them becomes a moral imperative. Here’s how Hospital Aliança in Brazil is doing it.
By: Eduardo Novaes de Carvalho, Cardiology Line Coordinator at Hospital Aliança; Bruno Battaglia, lean coach with Lean Institute Brasil; and Flávio Battaglia, Director of Lean Institute Brasil
The work of our hospital – which has 213 beds and 1,591 employees – is inspired and informed by our three guiding values – Excellence, Integrity, and Improvement. These were also the starting point of our lean journey, which was kicked off in May 2016 to improve the work of the Emergency Department.
The two main problems the hospital’s ER faced were: the lack of a dedicated flow for patients with chest pain and potentially suffering from acute myocardial infarction (AMI, commonly known as a heart attack) and a highly saturated flow of green patients, those low-priority cases who normally visit hospitals in large numbers.

With our guiding principles clear in mind, we were determined to study and tackle these two massive problems.
Green codes are the most frequent type of patient showing up at the ER, representing approximately 65% of the total volume of patients seen by the hospital. As a result, the long waiting time had a very bad effect on quality, safety, and patient satisfaction. Many patients even threw in the towel, deciding to discontinue care.
The Cardiology department also faced several challenges, the most visible being the overcrowding resulting from the mixing up of the flow of green patients and the flow of patients complaining about chest pain (sometimes mild, but still a potential sign of progressing AMI).
These dynamics created the impression across the local population that the ER of the hospital was not able to readily recognize and tackle AMI, causing dissatisfaction and leading several patients with suspected heart disease to not seek the hospital’s care anymore.
From a technological and professional standpoint, the ER is highly developed, with one of the best hemodynamic services (critical to angioplasty in the treatment of infarction) in the north-northeast of Brazil. Despite this, some of the performance figures for Cardiology were worrying, with low occupancy in the cardiac ICU (40% idle rate) and a 70% idle rate for the area overall. There were also problems with communication and the flow of information, and no standard to identify patients with chest pain and immediately call for an ECG (electrocardiogram) and follow-up.
The goal was to implement a more structured approach to providing care for AMI cases, based on a multi-professional protocol that aimed to better manage each point of contact with the patient (building on the high standard of care the hospital provides and the involvement of medical, administrative and reception staff). The first move was to identify the critical points that offered a greater chance of service failure, which necessarily meant monitoring and measuring processes using a set of quality indicators.
An example of the application of the new protocol is the indicator called Door-ECG, measuring the time interval between the arrival of the patient presenting chest pain at the hospital door and the first ECG performed. We determined this shouldn’t exceed 10 minutes.
Another important indicator is the Door-Balloon Time, which represents the time interval between the arrival of the patient with chest pain and the performance of the angioplasty to open the obstructed artery. In this case, the goal was maximum 90 minutes.
When the protocol was implemented (which would ensure a faster, more efficient, and safer flow of care), AMI-related performance was out of the target and over the times specified. (There was also a need for Hospital Aliança to conform to international standards for the care of infarction.) Yet, in a situation in which every single minute counts, bringing clarity to the AMI process became a necessity, as well as a moral imperative. There was a lot of hope that the protocol would have an impact.

HOW THE JOURNEY BEGAN
Using lean principles to meet its newly-found challenge, Hospital Aliança launched a Value Stream Improvement project.
To start off, two teams were created – one focused on the Cardiology value stream and another focused on the flow of green patients. Clearly, selecting and training the right people to form these teams was perceived as a very important task, because the success of a transformation largely depends on the commitment and engagement of those involved in it.
Team members were all healthcare professionals with no management experience, who were suddenly invited to join a world they didn’t know, made of indicators, goals, and action plans. Understandably, at first they appeared reluctant and scared. That’s when the importance of the role of top leaders in the hospital became clear: the Board saw in lean a great opportunity to turn those great front-line professionals into great leaders who would be able to ultimately transform the organization.
First of all, lean principles had to be assimilated by everyone involved. Following these training sessions, the hospital moved on to the first stage of its Value Stream Improvement project: the selection of the problem and the definition of the project’s scope. Because the greatest understanding of the problems lies with those who perform the work every day, a multidisciplinary discussion was initiated to get a more accurate idea of the difficulties the hospital would encounter and to identify the barriers that prevented it from achieving its objectives. Having different points of view coming from different areas is key to ensuring a more holistic and comprehensive understanding of the problem.
The practice of going on gemba walks was also introduced (they are much more impactful than many think). Hospital Aliança had three main goals for the walks: validating the problem identified in the current state; analyze opportunities for improvement using a multidisciplinary approach; and provide a format for building the desired future state.
As the walks started, the team began to feel much more confident about continuing the project, because they now had a much deeper knowledge of the problem at hand and a number of hypotheses and assumptions raised had already been eliminated or validated depending on what was observed at the gemba. They felt like they could move on to the next stage.
MAP, PLAN, ACT
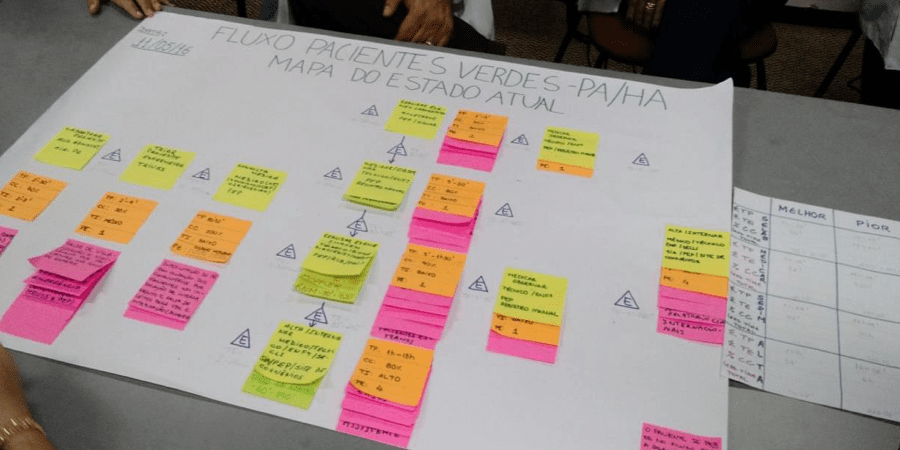
It all started – as it normally does in lean environments – with an A3, which was used to map the current state and, with that, see opportunities for improvement. The process was broken down into stages, which were then timed and searched for bottlenecks.
But mapping the current state is just the first step in building an A3: the analysis of the problem and elaboration of possible countermeasures followed, allowing the team to imagine and define their future state.
The cardiology team identified 15 causes for the problems that were generating waste and preventing the hospital from getting the best possible results. They divided them into five categories: Emergency problems, hemodynamic problems, cardiac ICU problems, hospitalization problems, and cardiac MR/CT problems.

The team proceeded to find countermeasures for each of the causes, using a suggestions system that involved all stakeholders and engaged everyone in solving the problems. Thanks to these countermeasures, it was also possible to draw the map of the future state. The team now knew where they wanted to go.

Meanwhile, the team focusing on the flow of green patients had also done its root-cause analysis. They drew a diagram revealing the reason for the long waits. Fifteen were identified, highlighting what caused the delay in each of the steps the green patient had to go through: registration, screening, medical consultation, examination, medication/observation, and discharge/hospitalization.

Just as the Cardiology team had done, the team gathered suggestions from all those involved and established countermeasures to deal with the problems and their causes once and for all. They too proceeded to draw their future state map.

Finally, both teams prepared an action plan to reach their desired future state, defining what would be done, according to each established countermeasure, who would do it, and by what deadline. (This action plan is at the end of an A3, after which the team agreed on how they would track results to see if further action was required.)
THE RESULTS
Today, Hospital Aliança has a more integrated system and better-connected teams. Everyone feels responsible for the success of the hospital and sees with greater clarity the different points of view of different areas of the organization, which in turn ensures there are more confidence and commitment in the decision-making process.
All the actions the hospital took have resulted in really positive results, and in a very short time. Between May and August 2015, before the start of the project, the hospital had cared for 18,974 patients, of whom 1,471 (7.7%) had stopped showing up to receive care. (Of these, 975 – mostly green and cardiology patients – reported the delay in care as the main reason behind their decision.)
In the same period in 2016, at the beginning of the lean implementation, these numbers had fallen by 70%, reaching a historic low of 439 (or 3.2% of the total number of patients). And of those 439, only 194 reported doing so due to service delay – a drop of 80% from the previous year.
Cardiology solved many of its problems through simple and creative standardized work, bringing increased agility to the provision of care.
The creation of a thoracic pain identification system (CODE 99) now goes into action as soon as the patient arrives at the hospital reception. This year, the average time between the patient's arrival at reception and the ECG is four minutes, whereas in 2016 (when the protocol didn’t exist yet) it exceeded the recommended 10 minutes. These days, the ECG is often done as soon as the patient enters the hospital since the system to signal priority enables the team to act immediately.
The time to perform the angioplasty for the treatment of AMI has also been reduced. Two more standards were introduced to reach this objective: the AMI KIT, to ensure all the material needed for the preparation of the angioplasty and all the indicated drugs were readily available, and the AMI KEY, whereby an icon is made available in the electronic medical record to include a patient in the protocol, alerting the laboratory and hemodynamics teams. The new system has resulted in a 23% reduction in the time between the arrival of the patient with chest pain and the angioplasty (from 112 minutes to 84 minutes, within the target of 90 minutes the hospital had set for itself).
The hospital has noticed an improvement in patient satisfaction (after all, nobody likes to wait and everybody has a right to excellent care), and achieved its goal of dramatically improving the emergency care of myocardial infarctions. When time is of the essence, lean seems to be just what the doctor prescribed.
For an interview with Dr Eduardo, click here
THE AUTHORS



Read more


CASE STUDY — Simon, a Spanish leader in electrical mechanisms, went from growth-fueled fragmentation and operational complexity to a coherent, people-centric lean system spanning factories and offices worldwide.


FEATURE – Aligning supply flows with demand is crucial to success, but it can be complicated. Lean Thinking can help us identify the strategy and sequence of activities that we need to make it a reality.


FEATURE – Faced with increased production volumes, this Dutch company realized the need to improve its processes by developing people skills.


FEATURE – They say lean is all about people, and yet emotions – something we all feel and express daily – are largely absent from the lean discourse. The authors discuss the role they play in a lean transformation.

