How a Medical Office catalyzed a lean healthcare turnaround
CASE STUDY – A physician tells PL the story of how the East Denver Medical Office became a catalyst for the lean transformation at Colorado Permanente Medical Group.
Words: Hanah N Polotsky, MD, MBOE, FACP, Colorado Permanente Medical Group – United States
When a patient called a regional call center in 2014 to get an appointment with his primary care physician at East Denver Medical Office – a one-stop outpatient medical clinic providing integrated services to a diverse population of 46,000 patients, including primary care, pharmacy, laboratory, medical imaging and limited specialty care – he spoke with several registered nurses and physicians. His electronic chart bounced between various staff members in the medical office, when in reality his medical problem could have been solved immediately by his physician, had he been directly connected to him.
Meanwhile, his physician was overwhelmed by the demanding volume of paperwork and electronic virtual patient care, which meant often working through lunch and staying an extra two to three hours after his regular office hours to catch up. He was in the process of interviewing for an internal transfer to a hospitalist job that would not require so much non-physician work. This is not an unusual occurrence in primary care or medicine in general in the United States: physician burnout, resulting in inefficient and often poor patient care, has been studied and eloquently presented in numerous medical and business articles.
At the time, I was new to Colorado Permanente Medical Group. I had been promoted into management as an Internal Medicine chief after only six months with the company. Throughout healthcare, physicians are often moved into leadership positions, not always because they are good at it, but because few are interested in taking on the additional demands and stress inherent in such roles. I was motivated to learn all I could about management and find a way to decrease burnout, while creating an enjoyable environment for physicians and staff alike and providing excellent and timely care to our patients. Luckily, my brother, a six sigma master black belt working in the pharmaceutical industry, sent me a copy of The Machine That Changed the World. This book changed my world, and this is how the lean journey began at East Denver.

Working closely with the East Denver Medical Office Director, Patricia Houlton, who has since retired, we set out to learn various successful lean management models in healthcare – more specifically, primary care. We looked at other Kaiser Permanente regions, the National Health Services in Great Britain, the Mayo and Cleveland Clinics, Thedacare, Intermountain Health, and many others. The research conducted by author and professor Thomas Bodenheimer, MD at the University of California San Francisco, defined successful primary care models that create “joy in practice” for healthcare professionals, while providing first-rate patient care. This research led us to Virginia Mason to study flow in primary care. The organization was at the forefront of lean in healthcare, and we spent three days there learning the basics of 5S, flow, standard work and value stream mapping. Their instructors challenged us to imagine our model and build a flow station (equivalent to a u-cell in manufacturing) right there and then.
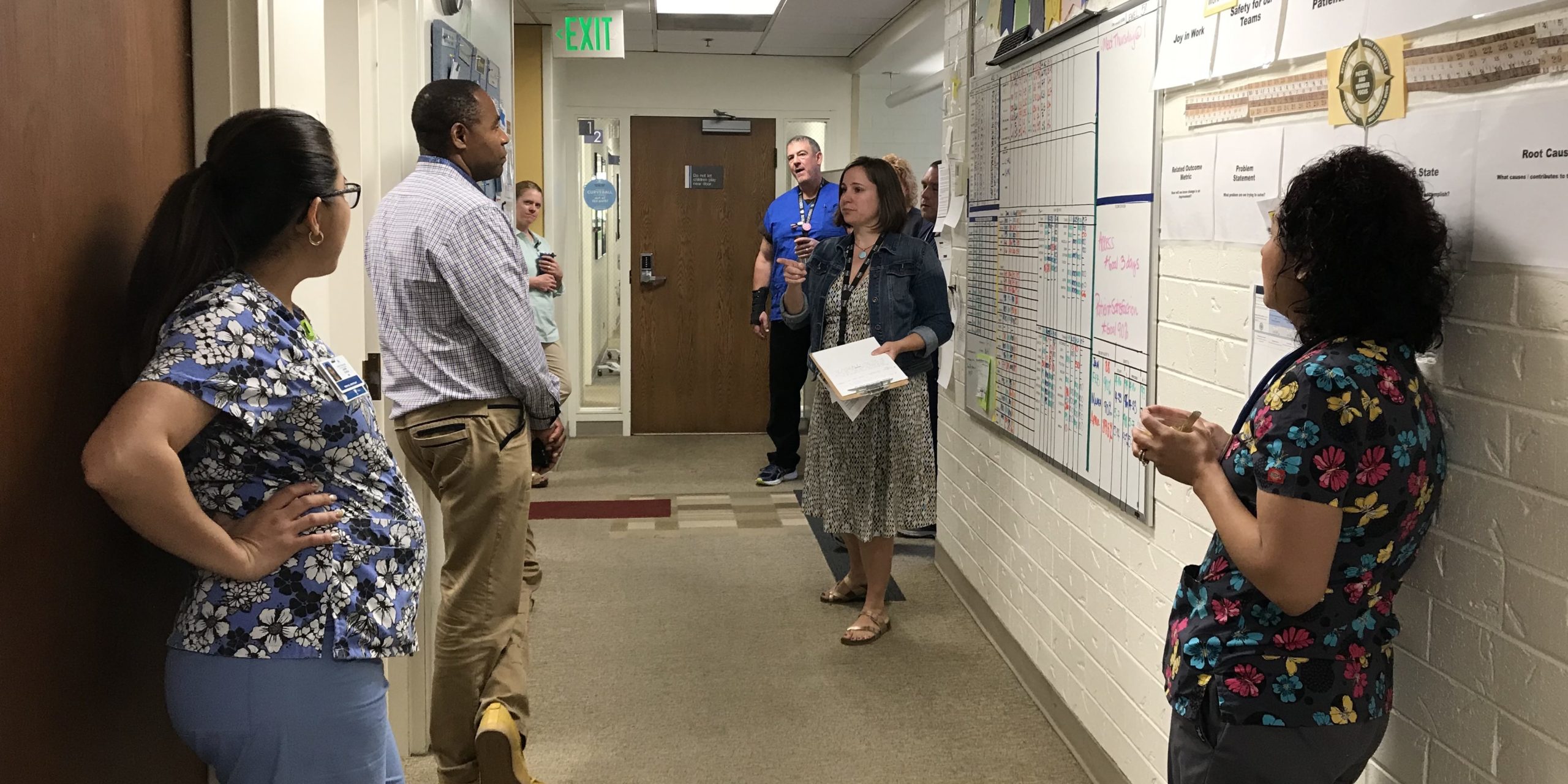
As often happens at the beginning of a lean transformation, we got back to work and started using the tools right away. We held a Rapid Improvement Event in November 2014 to teach the basics of lean thinking to physicians and staff. Physical and virtual patient flows were defined, silos were broken, and everyone refocused on patient care instead of blaming each other, as had often been the case in the past. The hierarchy was dismantled – executives and middle managers, physicians and their support staff started to see each other as partners in creating a perfect patient experience.
One of the most stunning revelations from the improvement event was the fact that each of the physicians on the team handled routine tasks differently, which created much variation in the daily work of their staff. For example, each physician had at least two or three ways of responding to test results. When multiplied by 15 physicians, result management created a lot of rework and defects.
This epiphany inspired physicians to standardize result management and become role models of workflow standardization to the rest of the staff. It is rare in lean healthcare transformations to involve physicians early in the process, because they are typically seen as obstacles to standardization due to their propensity for autonomy. In our experience, however, physicians who are engaged early on in visualizing and sharing their personal workflows will agree to simplify and standardize processes, to make it easier for the rest of the team to respond timely to patient needs.
Next, they agreed to standardize their exam room layout, including supplies and patient handouts. Many of these materials were outdated and often not even used, yet rooms were full of them. Following the layout improvement, the number of handouts placed in rooms decreased from more than 100 to 10. The same process took place with in-office medications and we reduced their number by 40%.

The first year following the RIE focused on two aspects of lean: 5S (room and workflow standardization) and daily continuous improvement through idea management (which was led by Jessica Weidner, a newly hired nurse manager, and Mehul Gandhi, MD, MBA, a new Internal Medicine chief). Our first Idea Board was simple, but proved to be a powerful tool to change from a culture of blame to one of problem solving. Managers walked around with idea cards in their hands and every time a physician or a staff member complained, they were given a card to fill out and encouraged to translate their complaint into a request or solution. Daily huddles were initially introduced for day-to-day operations and they quickly became problem solving and idea management huddles. Over time, as the number of ideas increased, the idea board and idea management process went through several iterations to ensure that the number of projects remained manageable and old projects were completed before new ones were started.
Physical and virtual workflows were simplified and standardized in the Training Within Industry (TWI) format. Front-line staff actively participated in standard work development with multiple iterations of each standard work process. East Denver leadership partnered with Unit-Based Teams ensuring collaboration and alignment between the Health Plan, the Medical Group, and Unions. Unit-based teams are similar to the quality circles that originated in Japan. To ensure sustainability of new standard work, nurses and medical assistants identified one of our most respected licensed practical nurses, Daniel Onyema, to transition into a coach role. Daniel learned the basics of coaching and TWI standard work development. A training grid was used to ensure that every current and new staff member was trained to standard.
The following year, we were ready to implement co-location of physicians and licensed practical nurses as well as registered nurses and medical assistants. Our goal was to create one-piece flow (or one-call resolution) as is more applicable to healthcare. A business case was presented to the executive team to request additional nurses support to ensure 1:1 physician-nurse staffing for co-location. At first glance, this seemed counterintuitive to lean thinking: lean usually results in increased capacity due to a decrease in workload and enhanced productivity. In Primary Care, however, with the introduction of the electronic medical record, physicians became bottlenecks of care, spending hours on tasks that did not require their expertise. In turn, this decreased the physicians’ direct interaction with patients to resolve problems in real time, which could prevent unnecessary urgent care and emergency room visits. We proposed that a small increase in licensed practical nurses support would result in more time and capacity for physicians to do “physician work” in real time as patient phone calls and e-mails come in. Physicians, freed from those non-physician tasks, now spend more time with their patients, during their visit, to anticipate future problems and obviate the need for additional future visits (rework) for problems that could be addressed immediately.
We were granted permission to pilot what we called the Flow Model in 2016. Kristin Banks, DrPH joined the East Denver team as project manager/improvement advisor. She learned lean on the job by working with us and later transitioned into the Medical Office director role. As a result of our lean efforts in 2015 and the Flow Model in 2016, the East Denver Internal Medicine department achieved drastic improvements in staff and physician engagement, significant patient satisfaction improvement, a 6% reduction in Emergency Room visits by patients and a 0.4% decrease in cost of care per patient, which historically had increased year over year.

The next step for us was to spread lean management to the rest of the departments at East Denver, including other Primary Care services (Family Medicine and Pediatrics), as well as other departments (Laboratory, Medical Imaging, Pharmacy, Ob-Gyn, and Optomentry). Kristin Banks as Medical Office director and I as Medical Office chief partnered with Unit-Based Team leaders, various department chiefs and managers as well as regional continuous improvement specialists, to map the East Denver patient experience from start to finish. This value stream map identified opportunities for improvement in patient navigation through the building, as well as physical and virtual handoffs between various departments. This multi-disciplinary group of front-line staff and leaders continues to collaborate to develop and implement workflow changes. For each process or workflow, we developed a “minimum viable product” (based on Lean Startup ideas), followed by implementation that continues iteration until the process moves from pilot to the standard work stage. As a result, patient satisfaction scores in the building as a whole improved significantly from 2016 to 2017, including satisfaction with coordination of care. Staff satisfaction scores also improved dramatically and were higher than regional scores across all categories.
Since the very beginning of our lean journey at East Denver Internal Medicine, each member of our management team has worked tirelessly to influence every leader and change agent that entered our building. We imagined and created East Denver to be a model cell for lean spread across the region. Enthusiastic, naïve, and at times opportunistic, we constantly worked to influence others to embrace lean thinking and develop a continuous improvement mindset. Because our team thrived on innovation and change, we agreed to numerous regional improvement projects and embraced every opportunity to share our lean experience and learning materials (from articles to books) with anyone willing to listen to us. Close to 300 executives, directors, middle managers, union leaders and front-line physicians and staff from medical offices and departments attended our “Intro to Flow and Joy in Practice” workshops at East Denver. Slowly, one by one, we successfully engaged our executives and peers.
At East Denver, we believe, as many healthcare organizations do, that lean management enables us to offer more affordable healthcare. We set out to bring quality into each physical and virtual patient encounter, eradicating rework and encouraging front-line problem solving and innovation. Each front-line healthcare team member is instrumental in helping us offer an outstanding experience to all our patients.
As leaders, we learned that lean is more about thinking and culture change, and less about tools. To our surprise, we learned that physicians, nurses, pharmacists, clerks, technicians and medical assistants aren’t opposed to standardization and continuous improvement, but actually come to embrace it when they see how it decreases their workload, streamlines their work processes, and helps to make the patient experience so much better. Contrary to a common belief, lean can be introduced and organically spread from the middle of an organization. However, this does require relentless hard work, front-line engagement, managing up, persistence, and willingness to fail and start over again, and again, and again.
THE AUTHOR

Read more


FEATURE – Pure and simple management by indicators can be a trap leading us to make decisions that are inconsistent with the real needs of a company. The balance between facts and data is key.


FEATURE – Tackling climate change forces us to rethink everything we do as a society. Here’s three lean lessons that can show us a way forward.


FEATURE – In this compelling read, the author explains how “centerlining” tools and settings can reduce variation in a process and avoid having to constantly seek adjustments à la McGyver.


FEATURE – Moving her assistant's workstation next to hers and introducing standardized work helped a family physician in California to provide better, faster care to her patients and to avoid burnout.

