Using lean to discharge patients before 12PM
FEATURE – This nurses-led experiment in Barcelona’s Hospital Clinic is proving successful in getting more patients discharged on time and avoiding surgery cancellations.
Words: The Orthopedic-Traumatology Surgery team
BACKGROUND
In the context of the economic crisis of 2008, as it struggled to address the high demand for knee replacement surgery and a long waiting list, our Unit took the opportunity to review its processes and introduce a new protocol, known as Fast Track (first used in Denmark in 2002).
Under this “Day 0” pre-hospitalization model, patients enter the ward on the same day their procedure is scheduled (they could be coming from outpatient care, for planned surgeries, or from the Emergency Department). The aim is to optimize the process and reduce the average length of stay, which notoriously has a huge impact on the cost of hospitalization, while maintain quality and patient satisfaction.

We recently found the protocol was no longer giving us the benefits we hoped – not surprisingly, given that in the meantime our processes changed significantly, and we even went through a pandemic. We were struggling to get post-operatory patients in our ward before 12PM, because beds were always occupied.
This led us to kick off a lean project called “Discharge before 12PM”, originally in the third trimester of 2019. The Covid-19 pandemic forced us to postpone time and time again, and we eventually started in earnest in February this year. We didn’t completely start from scratch: a similar project had been run in another area of our hospital, the Pneumology Department. Despite the differences between the two departments (namely, that we work with surgeons rather than physicians), their experiment gave us a solid methodological base to build on.
As a pilot, we ran an experiment in the G123 room, which is characterized by limited capacity (16 beds) and normally houses patients with planned knee replacement surgeries (among others, based on availability).
GETTING STARTED
Prior to project kick-off, we had gathered data on length of stay, discharge times, and main reasons for late discharge. Through this analysis, we found that in February 2020, around 20% of patients were discharged before 12PM, a percentage that dropped to 17.9% in September 2021 and to 9.1% the following month. With most patients discharged between 11AM and 4PM, this prevented “Day 0” patients who just got out of surgery from being brought up to our ward, leading to the cancellation of planned surgeries.

Armed with data, our first step was to organize meetings with a multi-functional team, to create a value stream map that would help us to identify the main pain points in the process.
These were the main problems we found:
- The doctor requests discharges and writes prescriptions in batches, with no specific time for doctor-nurse visits scheduled.
- Therapeutic education, which is critical for recovery, is provided on the day of discharge, right before discharge, usually after 12.
- We need to find the doctor responsible for the patient to get him or her to sign off the discharge, and only then can we request an ambulance to transport the patient to their home (it, therefore, always arrived after 12).
- To book an ambulance, the administrative person requires information from a nurse and/or physiotherapist.
- Nurses can’t prepare the discharge documents until a doctor authorizes them to. That means the work didn’t flow, because the upstream step in the process delayed the downstream one.
- Nursing assistants need to complete skin decontamination, a process that takes time during the morning shift, which means that the nurses’ workload is concentrated on the same day as the discharge.
Our goal with this lean project was to have at least 50% of our patients discharged before 12PM, starting in November 2021. The target was set based on the number of daily discharges in our unit and the need for free beds for patients coming from surgeries or the ER.
HOW WE DID IT
It all started with the observation of the current process at the gemba. We studied the tasks of each person contributing to the process and measured the time they need to complete them as they tend to each patient. With this data, we were able to create a diagram of precedence showing all the possible pathways to handle a patient.
On average, nurses need 30 minutes to prepare the discharge documentation and explain to each patient what therapy they need to follow during their recuperation. Hygiene and skin decontamination takes nursing assistants 20 minutes on average, whereas doctors require 15 minutes to prepare the necessary documentation and requests for outpatient care providers. On their part, it takes 18 minutes for physiotherapists to take the patient through the therapeutical exercises they will need to do at home. We saw an opportunity to save time here, by organizing group sessions to educate patients in the workshop room, but this wasn’t always available.
With 76% of the tasks to be completed on the day of discharge, it seemed impossible to discharge patients before 12PM. So, we decided to see which actions could be carried out the day before discharge. These refer to the observations on the problem we shared above, and included:
- Completing requests for external consultations, signing off rehabilitations, post-operatory tests and x-rays, and preparing prescriptions in the operating room after the procedure.
- Carrying out follow-up blood sampling at 11PM, during the night shift, rather than at 7AM the following day, to have the results during our morning rounds on the day of discharge.
- Having the administrative person contact the x-ray coordinator 24 hours after the operation to arrange a time, together with physiotherapists and/or nurses, to carry out the necessary x-ray exams.
- Requesting the checks for patients regularly taking anti-coagulants during our rounds.
- Scheduling ambulances the day before discharge for patients needing it, so they can leave before 11AM. This requires the nurse or physiotherapist to communicate effectively with the administrative worker, so that they can arrange for a wheelchair or stretcher.
These changes meant that we now had to complete only 40% of tasks on the day of discharge (down from 76%), which led to improved results in discharge times.
To support our new way of working, we developed a number of tools. First of all, we introduced a checklist for each professional category (nurses, administration, nursing assistant, physiotherapists, doctors, and social workers), guiding them through the tasks that need to be carried out during a patient’s stay. This proves particularly helpful when it comes to onboarding people who are new to the ward, which traditionally experiences high turnover. Of course, the checklist is accompanied by word of mouth: we try to get new people to interiorize our way of working as quickly as possible.
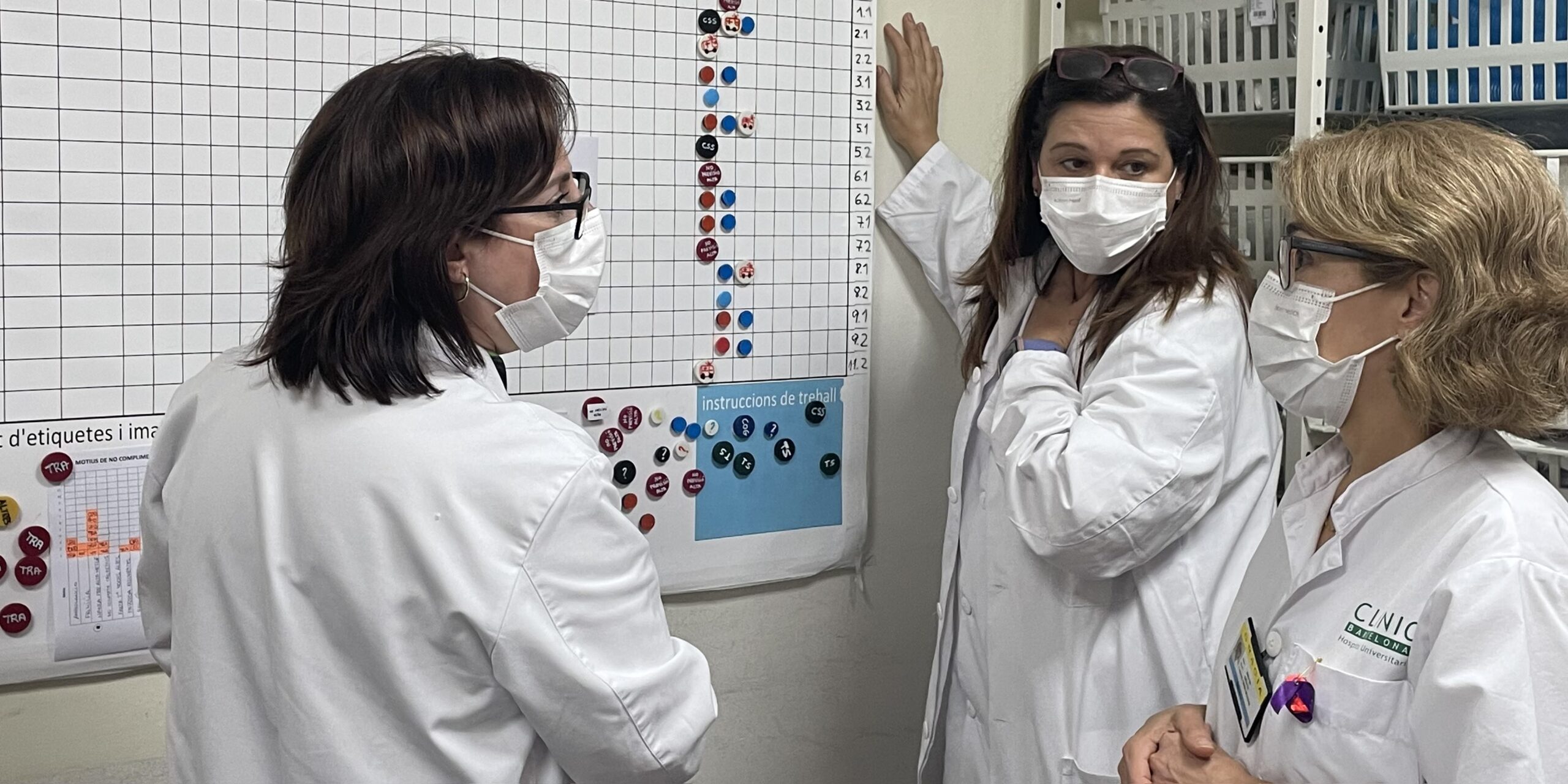
We also introduced two visual boards, one offering an overview of the day’s expected discharges and one on the status of our beds. The discharge board carries information on the process as it pertains to the day before discharge and the day of discharge, for each of our 16 beds. It informs all those engaged in the discharge process, telling the doctor, nurses and administrative worker what patients are to be discharged, so that all the necessary arrangements can be made, and documentation prepared. In turn, the beds board uses a simple traffic light system to visually and immediately show the nursing assistant, the cleaning staff and the administrative worker which beds are dirty (red), clean (yellow), or ready for a new patient (green). Providing people with this data prevents us from wasting time looking for the right people to confirm whether a bed is available when we receive a call from Surgery that a patient is ready to come up. The work flows better these days, and it all happens without the need to utter a single word!
Since starting the project, we have been gathering data every week. We record the evolution of discharges and the times of discharge (using a Pareto chart). We also highlight the reasons a patient couldn’t be discharged before 12 and outline the actions we propose to solve the issue. Little by little, we attack the problems we highlight on the board, and the effect can be felt across the process.
Recently, for example, we mentioned to doctors the problem of not having pre-discharge documentation ready on time. They talked about it and decided to always provide the on-call doctor or resident with a pager. This helps the nursing staff, because they know that whatever problem they may encounter between 9AM and 12PM, a doctor will be around to help them speed things up.
The board boosts engagement, too, because nobody likes to see a red result on it and people now understand how that red affects everyone’s daily work. We are gradually “spreading the word” about what we are doing with lean, by engaging more closely with people from other wards that we find ourselves working with. It’s great to see that, once we tell them what we are trying to do, they are typically very happy to participate.
To make everyone aware of the trend of discharges even when they can’t participate in the meeting, we make a point of emailing the data to the whole team. We are also holding weekly follow-up meetings (every Monday), during which the whole team discusses results and countermeasures. In the graph below, the most common problems preventing us from meeting our objective.

RESULTS
While we don’t always reach our 50% goal, a lot of time we do. We might never achieve 100% (patient safety comes first and is always more important than our internal process), but it’s a good objective to aim towards. We are certainly on the right track to gradually even out the trend and achieve stability and consistency in the discharge times. This is possible because the whole team is engaged and wants this to work. We were pleasantly surprised by the level of engagement of surgeons: naturally, they spend more time in the OR than in our ward, so it’s great to see how much they are getting involved in a nursing-led project. They have understood that the whole process stops if they don’t provide the pre-discharge documents, and they have changed their behavior accordingly.
Looking forward, our main goal is to avoid losing speed. With the frequent turnover of staff (we get new residents in the unit every month, for instance), this has happened occasionally, but we are confident that by engaging more and more people and solidifying this way of working as our standard we will not experience the same problem.

We have learned a lot from this lean experiment. In particular, we recognized the huge importance of observation in taking our first steps and truly understanding the situation we found ourselves in. We also think it’s been critical to work with a multi-functional team, a cross-section of the process, and to standardize tasks so that everyone works in the same way, and it becomes easier and faster to teach new people.
The reason lean is working for us is that it defined and even celebrated the contribution of each and every team member – from cleaning staff to surgeons – to the overall success of the area. Discharging patients before 12PM is a problem common to most public hospitals, and we hope our experience can inspire others to tackle it using lean.
THE AUTHORS

The whole team is working hard at this project and participated in the creation of this article. Thank you to all: Gracia Ginés, Rosa Marina, Agnes Nicolau, Anna Voltes, Montserrat Monfort, Raquel López, Aroa Herrero, Ana Alicarte, Jorge Fernández, Laura Heredia, Josep Maria Segur, Juan Carlos Martinez Pastor, Marta Sabater, Montse Nuevo, Montse Linares, Carol Gascueña, Irene Alonso, Andrea Vigueras and Pilar Camacho.
Read more


FEATURE – Lean is a people-centric system for learning that acts as an alternative to traditional management and financial capitalism. It represents the best strategy a company can adopt to meet the needs of the future.


FEATURE – The successful project discussed in this article shows how Lean Thinking can bring huge benefits to small and medium enterprises and paves the way to a new way of looking at lean coaching.

WEB SERIES – Episode 3 of our docuseries on lean in Brazil takes us to the second largest bank in the country. Learn how Bradesco is striving to improve its processes to provide more value to its customers using Lean Thinking.


NOTES FROM THE GEMBA – This French company has completely transformed its approach to designing and introducing new products to market by embracing lean product development ideas.

